New research presented this week at ACR Convergence 2022, the American College of Rheumatology’s annual meeting, demonstrated an association between age of diagnosis and clinical characteristics and treatments in Anti-neutrophil cytoplasmic antibody-associated vasculitis patients.
Anti-neutrophil cytoplasmic antibody-associated vasculitis (AAV) is a group of conditions characterized by the development of autoantibodies to the neutrophil proteins proteinase 3 (PR3-ANCA) or myeloperoxidase (MPO-ANCA), leading to systemic inflammation and damage to small blood vessels. AAV includes granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA) and eosinophilic granulomatosis with polyangiitis (EGPA).
As stated in the abstract, although clinical characteristics and outcomes often differ between children and adults with the same rheumatic condition, comparative data is limited in AAV. The goal of this study was to examine the relationship between age of diagnosis and disease characteristics, treatments, and damage in AAV patients.
The retrospective cohort analysis included 1,020 patients with GPA and MPA enrolled in the Vasculitis Clinical Research Consortium Longitudinal Studies from 2013 to 2021. EGPA patients (357) were analyzed separately. Participants were divided by age at diagnosis: children (under age 18), young adults (ages18-40), middle-age adults (ages 40-65) and older adults (over age 65). Children and young adults with EGPA were combined in a single category due to the small sample size (n = 87).
In the main cohort, 852 patients (84%) had GPA while 165 (16%) had MPA. Most were ANCA positive at diagnosis: 637 (65%) with PR3-ANCA, 247 (25%) with MPO-ANCA and 9 patients (1%) with both.
More females than males were diagnosed with AAV in all age groups; however, the difference was greatest when diagnosed in childhood and lessened with each progressive age group. Patients diagnosed as children were more likely to have GPA and be ANCA/PR3-ANCA positive while the amount with MPA and MPO-ANCA increased with age, further reflecting differences in AAV based on age at diagnosis. Symptoms also varied among age groups.
“In general, the child and young adult groups had more ear, nose, and throat (especially nasal septal perforation and subglottic stenosis), gastrointestinal, diffuse alveolar hemorrhage, and renal manifestations. The older diagnosis groups had more cardiac and nervous system manifestations than the younger diagnosis groups and experienced fewer musculoskeletal, cutaneous, ocular and sinus manifestations,” says Jessica Bloom, MD, MSCS, a pediatric rheumatologist and assistant professor of pediatrics at Children’s Hospital of Colorado and the study’s lead author.
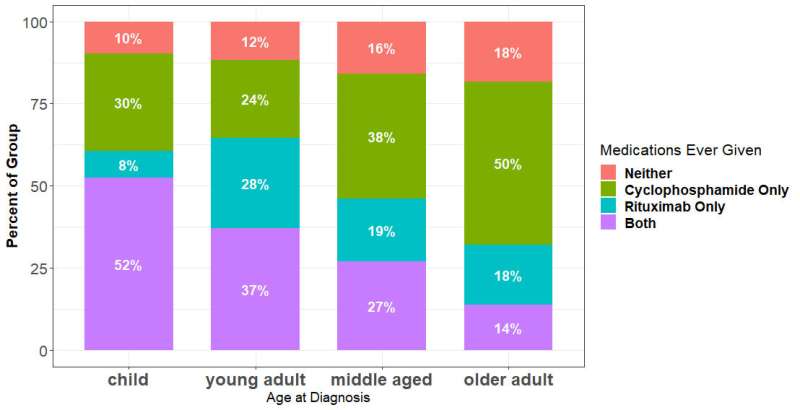
Over half of patients diagnosed in childhood received both cyclophosphamide and rituximab, whereas the percentage of patients receiving cyclophosphamide alone or neither drug increased with older age at diagnosis.
“Since submitting our abstract, we looked further into the data and divided medication use before and after 2012, since rituximab was approved for use in GPA and MPA in 2011,” Dr. Bloom says. “For GPA and MPA, we saw a significant difference in the types of medication used before and after 2012 for the child, young adult, and middle-age groups. This was specifically seen in the proportion of patients using rituximab only. For EGPA, the only difference was in the middle-age group, where the use of cyclophosphamide only decreased substantially and use of rituximab only increased.”
Dr. Bloom says the study didn’t look at the reason for these differences. But she points out that it is challenging for pediatric rheumatologists to apply research results from adult patients to pediatric patients because children may metabolize medications differently and present with different patterns of organ involvement.
The study also found that patients diagnosed after age 65 had significantly higher Vasculitis Damage Index (VDI) and ANCA-Vasculitis Index of Damage (AVID) scores compared to those diagnosed in childhood.
But Dr. Bloom says some components of damage scores used to study AAV reflect age-related damage rather than damage from the disease itself.
“Since submitting the abstract, we have created what we believe to be a more disease-related damage score by combining factors from both VDI and AVID that are more specific to the disease, rather than aging. After applying these analyses to the age cohorts, we no longer saw the statistically significant differences noted in the VDI and AVID analyses,” she says.
Overall, Dr. Bloom says the study is “a comprehensive analysis of a North American cohort of ANCA-associated vasculitis that demonstrates the ability to use adult registry data to analyze patients diagnosed in childhood, an important approach given the lack of rigorous research studies involving pediatric patients. [At the same time], there is a need for increased research involving children with AAV, which would allow for more evidence-based care and improved outcomes.”
More information:
Conference abstract
Source: Read Full Article
