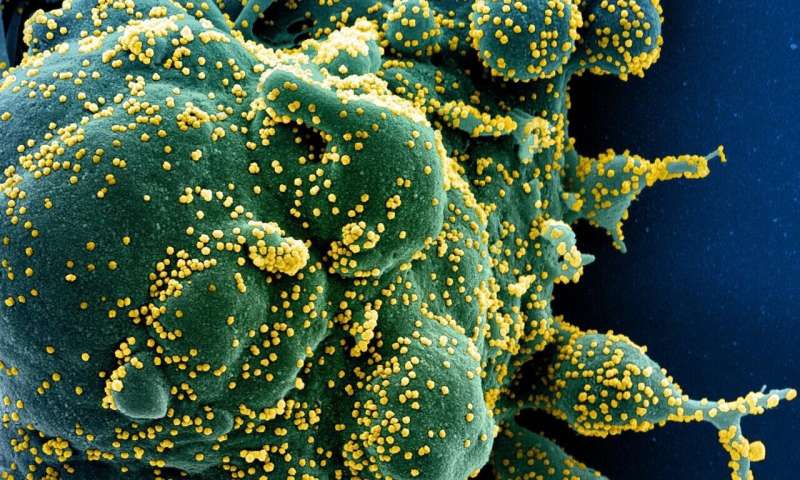
Researchers at the Francis Crick Institute and University College London Hospitals NHS Foundation Trust (UCLH) have studied whether antibodies produced as a result of infection with one SARS-CoV-2 variant are able to bind to and neutralize other variants.
Over the course of the pandemic, various COVID-19 variants have arisen with the Delta variant currently dominant in the UK. Understanding how some variants may be able to trigger an effective antibody response against other variants, in addition to itself, could help inform future vaccine design.
In their study, published in eLife (29 July), the scientists analyzed blood samples collected from patients who had previously been infected with COVID-19 and who were admitted to UCLH for other reasons, samples from health care workers as well as samples collected from patients at different points earlier in the pandemic. They identified COVID-19 antibodies in the blood, and in the lab ran tests to see if antibodies produced after infection with one variant were able to bind to and neutralize other variants.
The study included:
- The original strain first discovered in Wuhan, China
- The dominant strain in Europe during the first wave in April 2020 (D614G)
- B.1.1.7, the variant first discovered in Kent, UK (Alpha)
- B.1.351, the variant first discovered in South Africa (Beta)
While antibodies produced by one variant were able to bind to other variants at a similar rate, there were some differences in whether antibodies could neutralize other variants. If an antibody is able to neutralize a virus, this means it can stop the virus from entering the hosts cells in order to replicate.
The researchers found that antibodies produced by the Alpha variant were not able to neutralize the original or D614G strains as effectively, in comparison to neutralizing the Alpha variant itself.
Antibodies produced against infection with the D614G strain were able to neutralize both the Alpha and original strains to a similar level as D614G.
Both the Alpha and D614G strains produced antibodies which were not able to effectively neutralize the Beta strain.
There are many elements of the immune system which impact how protected an individual may be against future disease. This includes memory B cells and T cells which equip the immune system to deal with evolving threats. As a result, these findings do not necessarily mean people who were infected with specific variants are less protected against others.
Kevin Ng, co-first author and Ph.D. student in the Retroviral Immunology Laboratory at the Crick says: “It’s important to note that most people who have been infected with the virus will not know which variant they were infected with and it is critical that everyone eligible for the vaccine takes up the opportunity because we know they are effective in some way against all known variants.”
As the antibodies were able to bind to other variants at a similar level, but had differing ability to neutralize other strains, this suggests that there are only a few regions on the spike of the virus which are important to this neutralization process. It is the mutations within these key sites which impact the ability of antibodies produced by one variant to neutralize another.
Nikhil Faulkner, co-first author and Ph.D. student in the Retroviral Immunology Laboratory at the Crick says: “As the pandemic continues and more variants may arise, research into how infection with one variant impacts immune responses to other variants is important.
Source: Read Full Article
