The three co-inventors of optical coherence tomography — James Fujimoto, MD, PhD, and Eric Swanson, MD, of the Massachusetts Institute of Technology, and David Huang, MD, PhD, a professor of ophthalmology at Oregon Health and Science University — have received the 2023 Lasker-DeBakey Clinical Medical Research Award, the Lasker Foundation announced.

Dr James Fujimoto
Considered one of the most prestigious prizes for biomedical research, the Lasker Awards honor individuals who have “made major advances in the understanding, diagnosis, treatment, cure, and prevention of human disease.” The award is one of three the Lasker Foundation gives annually to innovators in medicine. Lasker prizes are sometimes referred to as “America’s Nobels.” Ninety-five Lasker award winners have gone on to receive the Nobel Prize, according to the foundation.

Dr David Huang
Optical coherence tomography (OCT) “revolutionized ophthalmology — allowing rapid detection of diseases of the retina that impair vision,” according to the Lasker Foundation. The imaging technology has evolved into a cornerstone of ophthalmologic practice since Fujimoto, Swanson, and Huang introduced it in 1991.

Dr Eric Swanson
“I’m very pleased that the Lasker foundation is bringing attention to optical coherence tomography, which has found really widespread use in ophthalmology,” Huang told Medscape Medical News. “I think it’s going to find even broader use in ophthalmology and also in cardiology and medicine in general, so this is great time for more people to know about it.”
Applications in Ophthalmology, Cardiology
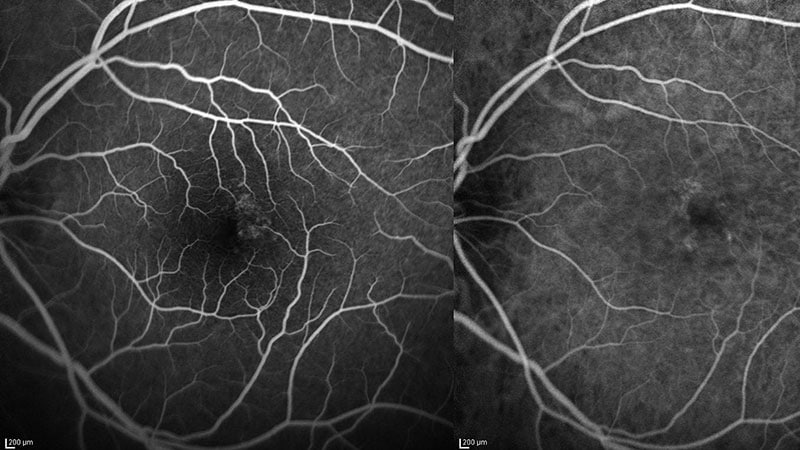
In ophthalmology, OCT has applications in scanning the retina to predict and diagnose retinal diseases such as age-related macular degeneration (AMD) and diabetic retinopathy, and it can scan the optic nerve and nerve fiber layer to track damage from glaucoma. The imaging test enables eye-care providers to identify vision-threatening disease early on, often before patients manifest signs and symptoms. In 2017, Swanson and Huang co-authored a study that reported that OCT had saved Medicare and AMD patients $11.2 billion from 2008 to 2015 by enabling personalized treatment with anti–vascular endothelial growth factor drugs.
Huang told Medscape that more than 40 million OCT images are captured in ophthalmology practices worldwide yearly. It has become the most commonly used diagnostic procedure for managing glaucoma, he added.
In cardiology, OCT can be used to characterize the composition of artery-blocking plaque, Huang said, with at least a 10 times’ greater resolution than even the highest-frequency ultrasound. “It can assess the risk of plaque rupture by looking at the composition of lipid, and it can guide stent placement and assess long-term outcomes,” he said.
“Revolutionary” Technology
“When we describe a technology as ‘revolutionary,’ it brought about a fundamental and significant change and transformed a field or the society. That is exactly what OCT has done to ophthalmology, especially in retina,” Judy E. Kim, MD, a professor of ophthalmology at the Medical College of Wisconsin in Milwaukee and president of the American Society of Retina Specialists, told Medscape.
“By providing high-resolution cross-section and enface images of the retina, as well as vasculature with OCT angiography, in a rapid and noninvasive manner that is user and patient friendly, we can diagnose diseases and monitor treatment effects in a personalized manner with improved accuracy,” Kim said. “OCT has also improved our understanding of disease progression and pathophysiology.”
She called OCT “an indispensable imaging tool” not only in patient care but also in clinical trials and basic and clinical research. “If I could have only one imaging tool in my practice, I would choose OCT,” Kim said.
Origins of OCT
OCT arose from Fujimoto’s work in the 1980s with ultrashort lasers. He had assigned Huang, then an MD-PhD candidate at MIT, to explore interferometry with short-coherence light to match the ability of femtosecond laser optics to distinguish skin layers and measure corneal thickness in animal eyes. Huang came up with a method, but the process was too slow to use in humans.
Meanwhile, at MIT’s Lincoln Laboratory, Swanson was working on intersatellite laser communications and high-speed fiber-optic networks. Fujimoto brought Swanson onto his research team, where they merged their concepts to create a high-speed, high-resolution method of imaging into a more compact platform.
“The development of OCT required a multidisciplinary community of scientists, engineers, and clinical thought leaders, with a partnership spanning government, academic, industry, and medicine,” Fujimoto told Medscape.
OCT in the Future
“In the future, it should be possible to have an automated OCT eye exam in your local drug store,” Fujimoto added. “Disease could be detected at an early treatable stage before irreversible loss of vision occurs. This promises to have a powerful impact on public health.”
Huang predicted the use of OCT will extend to other organs and larger targets. Previous iterations of OCT could image only a few millimeters of tissue because its resolution was so dense. The speed at which OCT can capture images has doubled every 3 years, and it shows no letup, Huang said.
“That’s going to extend its reach and applications,” he said. “And also because we can see the ocular circulation so well now with OCT angiography, by extension, we will be able to measure the health of the whole vascular system and also the brain; it’s a window into neurological conditions and cardiovascular diseases.” Advancements in computer technology and artificial intelligence are poised to push the limits of OCT even further in medicine, Huang said.
Huang has relationships with Visionix, Intalight and Cylite. Kim has relationships with Notal Vision, Heidelberg Engineering, and Optos.
Richard Mark Kirkner is a medical journalist based in the Philadelphia area.
For more news, follow Medscape on Facebook, X, Instagram, and YouTube.
Source: Read Full Article