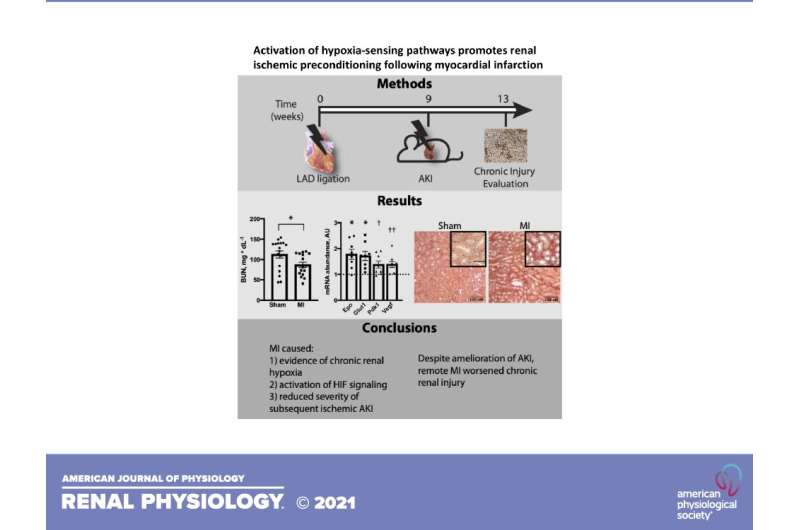
Scientists studying the effects of heart attack on kidney function recently made an unexpected discovery: Heart attacks actually provide short-term protection for the kidneys from subsequent acute injury. In a new mouse study, researchers report that oxygen content was reduced and activation of pathways sensitive to a lack of oxygen were stimulated in the kidneys after a heart attack. The research team also found that the protection seen in the kidneys post-heart attack was similar to protection observed in a separate group of animals that had healthy kidneys, yet were exposed to lower oxygen content in the air. The research paper has been chosen as an APSselect article for April.
Over time, however, the scientists reported that all of the initial protections of the kidneys evaporated and kidney function actually worsened as it relates to chronic kidney injury. The later results are similar to what is seen in patients suffering from both a heart attack and chronic kidney disease instead of kidney disease alone, according to the research team.
“It adds another layer of evidence that these pathways that we see are being protective in the short-term are probably very important,” said study co-author Andrew Terker, MD, Ph.D., of Vanderbilt University Medical Center in Nashville, Tennessee. “If we can figure ways to target that pathway, it could help treat or prevent these types of kidney problems in patients.”
The most common causes of kidney disease are type 2 diabetes and high blood pressure, Terker said. Researchers are hopeful the findings in this study will lead to new therapies to treat people with coexisting heart and kidney disease.
“Activation of hypoxia-sensing pathways promotes renal ischemic preconditioning following myocardial infarction” is published in the American Journal of Physiology-Renal Physiology.
https://youtube.com/watch?v=tpy20D-v5g8%3Fcolor%3Dwhite
Source: Read Full Article
