University at Buffalo researchers have discovered how an active form of a gene present in 75% of the human population works to protect the brain against neurodegeneration.
Published online in July in eBiomedicine and highlighted online this week, the findings provide insight into how the active form of CHRFAM7A helps strengthen brain structure in a way that is neuroprotective against diseases such as Alzheimer’s disease.
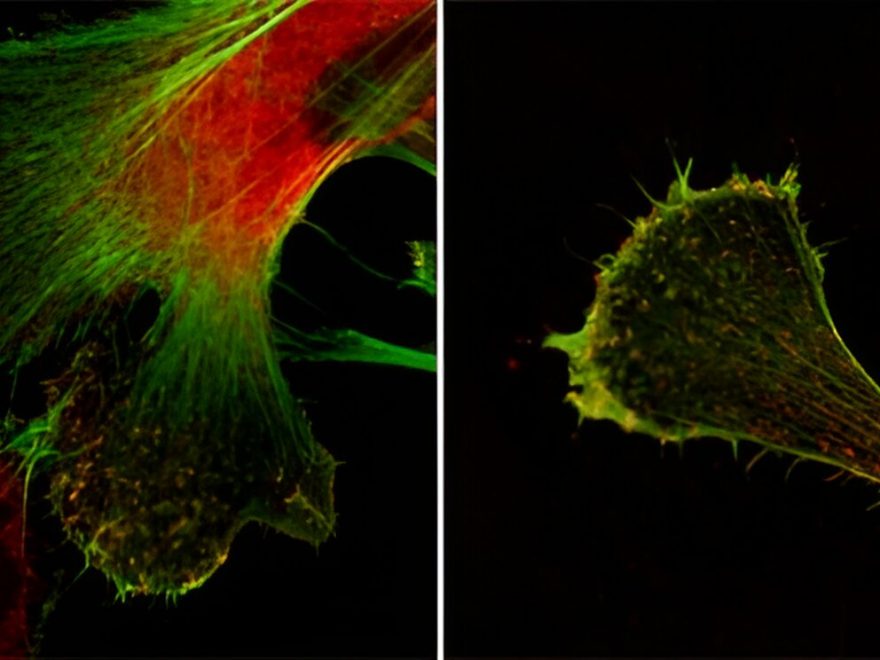
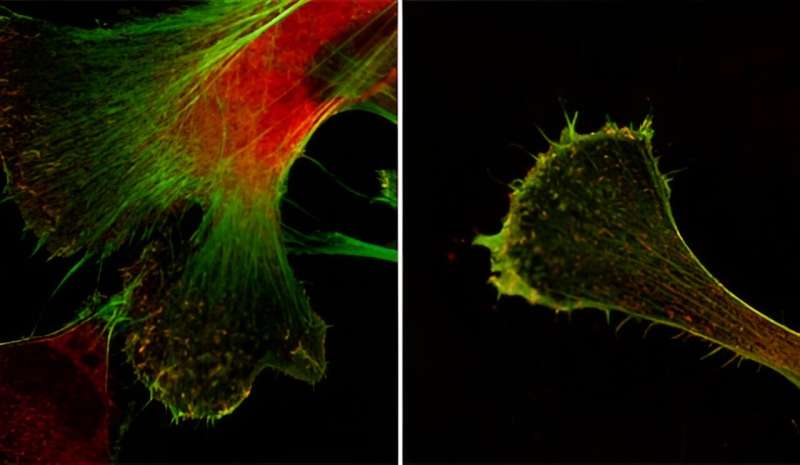
The study found that the active form of the CHRFAM7A gene activates the actin cytoskeleton, which provides structural support to cells, thus helping to make brain cells more resistant to stiffness, essentially becoming more flexible.
“Actin acts like beams in a house. It provides support for the cells in the cytoskeleton, which is the frame of the cell,” says Kinga Szigeti, MD, Ph.D., corresponding author, professor of neurology in the Jacobs School of Medicine and Biomedical Sciences and a physician with UBMD Neurology. “For the 75% of people who have the active version of CHRFAM7A, it may allow neurons to build stronger connections and to better adapt to changes in the brain environment.”
The gene, CHRFAM7A, is a fusion of a gene that codes for the Alpha 7 receptor for acetylcholine, a neurotransmitter involved in memory and learning, and long associated with Alzheimer’s and a kinase, a type of enzyme.
Three-quarters of the population has the active version while a quarter of the population does not. And it’s only present in humans, not animals, which, Szigeti explains, is why animal models of Alzheimer’s disease and other neurodegenerative diseases often don’t accurately predict how drugs will function in humans.
CHRFAM7A has also been implicated in many neuropsychiatric disorders, such as schizophrenia and bipolar disease.
“In this paper we show that this gene makes human brain cells develop stronger connections,” explains Szigeti, who is also director of UB’s Alzheimer’s Disease and Memory Disorders Center.
“It’s a very interesting conundrum,” she continues. “If you don’t have CHRFAM7A or you have less of it, you are at higher risk of developing Alzheimer’s disease because the brain is less structurally solid. But if you do have the active form of the gene, the drugs that we have now may not work as well because the Alpha 7 receptor for acetylcholine—which is what most drugs target—is altered.”
Szigeti says that the whole reason behind conducting this study was that there’s a translational gap in a lot of the very important genes affecting humans, especially those implicated in Alzheimer’s disease and psychiatric disorders.
“Neuroscience research has been overwhelmingly based on animal models,” she says, “but these diseases affect higher cognitive functions that are specific to humans and not present in mice, for example. This work is helping to fill in that translational gap.”
To do the study, the researchers developed human-induced pluripotent stem cells taken from the skin of adults who had Alzheimer’s disease and transformed them into neurons, creating essentially brain cells in a dish.
More information:
Kinga Szigeti et al, Neuronal actin cytoskeleton gain of function in the human brain, eBioMedicine (2023). DOI: 10.1016/j.ebiom.2023.104725
Journal information:
EBioMedicine
Source: Read Full Article