A new pathologic scoring system that accurately assesses how much lung tumor is left after a patient receives presurgical cancer treatments can be used to predict survival, according to new research led by investigators at the Bloomberg–Kimmel Institute for Cancer Immunotherapy at the Johns Hopkins Kimmel Cancer Center and the Mark Foundation Center for Advanced Genomics and Imaging at the Johns Hopkins University.
The study shows that pathologic assessment of residual viable tumor (RVT) in patients treated with immunotherapy and chemotherapy before lung cancer surgery provides a robust and efficient evaluation of patient treatment response that may be useful to guide patient therapy and predict survival. This latter finding supports pathologic evaluation of tumors as an early clinical trial endpoint and a surrogate of survival for potential accelerated regulatory approvals.
The results were published in the journal Nature Medicine and simultaneously presented by senior study author Janis Taube, M.D., M.Sc., director of the Division of Dermatopathology at the Johns Hopkins University School of Medicine and a member of the Kimmel Cancer Center, at the Society for Immunotherapy of Cancer annual meeting in San Diego.
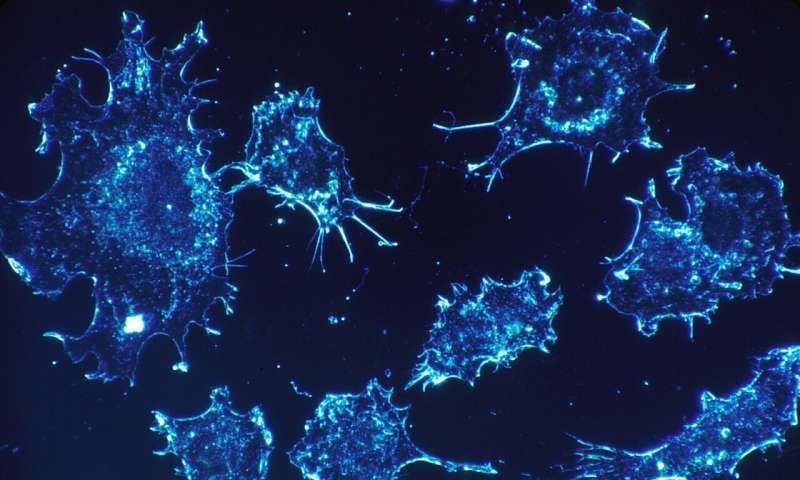
Immunotherapies harness a patient’s immune system to target their tumors. These powerful drugs are often paired with conventional chemotherapies to help shrink a patient’s tumors before surgery, increasing the likelihood of successfully eliminating the cancer. To gauge treatment success, oncologists typically rely on radiologic imaging of the remaining tumor, but the results aren’t always as accurate in early-stage tumors as they are for more advanced cancers.
More recently, circulating tumor DNA (ctDNA) clearance, which uses genetic sequencing to detect lung cancer-associated mutations in patient blood samples, has also shown promise, but is not yet widely available.
For the new study, investigators performed a new analysis on data from the randomized, phase 3 CheckMate 816 study. That study found that treating presurgical non-small cell lung cancer patients with immunotherapy (nivolumab) plus chemotherapy improved event-free survival. This important surrogate endpoint can help predict long-term survival and pathologic complete response, which measures whether any tumor is left.
“Most studies have focused on whether you have no tumor left or less than or equal to 10% of the tumor left, which is called a major pathologic response,” says lead study author Julie Stein Deutsch, M.D., an assistant professor of dermatology at Johns Hopkins.
During the study, the investigators used a new approach, which measures residual tumor in patients who received neoadjuvant therapy, to predict outcomes in patients with a greater range of treatment responses. They used immune-related pathologic response criteria (irPRC) to look for pathologic changes that indicated the tumor had been present in the tissue before immunotherapy but was destroyed by the treatment, allowing them to measure what percentage of the tumor was left, or the RVT, ranging from 0% to 100%.
As a result, they were able to separate patients into three groups based on how much tumor was left. In the future, data such as these may help guide the next round of clinical trials and ultimately help oncologists decide how to treat individuals in these subgroups, Deutsch says.
For example, patients with no tumor left may be able to skip postsurgical immunotherapy or have a relatively limited amount, while individuals in the intermediate group may need to continue immunotherapy for longer. Those who showed a very limited response may need to switch to a new therapy or add a new therapy to their regimen. The team’s next steps will include identifying the most clinically meaningful cutoffs for RVT.
They also looked beyond the primary tumor and used RVT to assess the immunotherapy effect on tumor in the lymph nodes, which showed additive value with the primary tumor for predicting survival. Long term, it may also be possible to strategically combine pathology, radiology and ctDNA results for the longitudinal monitoring of treatment efficacy.
Already, the investigators demonstrated the pathologic scoring system can assess 10 types of tumors, including lung, skin and colorectal cancers, which could be another advantage over other tumor scoring systems.
“The common features seen across these multiple tumor types means that pathologists don’t have to switch to different scoring systems for assessing pathologic response. This is similar to what already exists in radiology, where the RECIST system is used across all tumor types for determining objective response to therapy,” Taube says, noting that pathologists already are completing the necessary workflows as part of standard procedures when assessing surgically removed tumors.
Assessing RVT is inexpensive and uses tools and supplies commonly used by pathologists, Deutsch says, which may also make it accessible for those working in low-resource settings.
“It is important that as these immunotherapies move into clinical trials and become standard of care, pathologists worldwide have a standard scoring system for the assessment of treatment response,” Taube says.
More information:
Julie Stein Deutsch et al, Association between pathologic response and survival after neoadjuvant therapy in lung cancer, Nature Medicine (2023). DOI: 10.1038/s41591-023-02660-6
Journal information:
Nature Medicine
Source: Read Full Article
