New research from an immunology team at the University of Chicago may shed light on the challenges of developing a universal flu vaccine that would provide long-lasting and broad protection against influenza viruses.
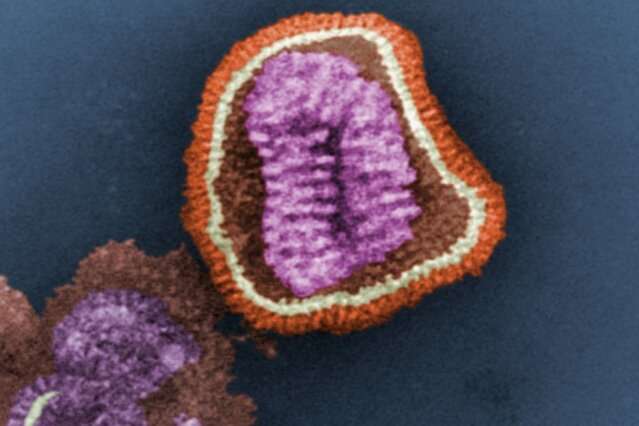
The study, published October 22 in Immunity, explores the behavior of polyreactive antibodies—antibodies that are capable of binding to more than one distinct antigen—in an effort to understand their role against influenza viruses. The researchers identified that broadly neutralizing antibodies are commonly polyreactive and are preferentially induced by novel and pandemic-level influenza viruses.
The research is inspired by the limited efficacy of the annual flu vaccine, which must be adjusted each year to provide the best protection against commonly circulating strains of the virus, and why it so rarely induces broadly neutralizing antibodies.
“For whatever reason, when we are exposed to the flu virus, the antibody response mounted targets the parts of the virus that want to change, so you have to get vaccinated every year to keep up,” said Jenna Guthmiller, Ph.D., a postdoctoral fellow at the University of Chicago. “But there are some parts of the virus that don’t change. So why doesn’t the seasonal flu vaccine produce antibodies that target those?”
This study has implications for the development of a universal flu vaccine that can elicit broadly neutralizing antibodies and that would only need be administered once or twice during a person’s lifetime, instead of every year.
These polyreactive antibodies, like all antibodies, are produced by the body’s B cells. When a person receives their annual flu vaccine, B cells will bind to the inactivated virus and begin generating antibodies against it, preparing the body to fight off the pathogen if it encounters the live flu virus in the environment.
This vaccine-induced immune response tends to produce very specific antibodies that target those frequently-changing epitopes on the surface of the virus, in contrast to broadly neutralizing antibodies that can identify the conserved regions that are the same every year.
It’s not clear why these polyreactive antibodies aren’t produced by the annual vaccine.
“Our research is trying to understand the features of broadly neutralizing antibodies, and why they’re so rarely induced by the seasonal flu vaccine,” said Guthmiller. “In this case, we were interested in understanding what gives polyreactive antibodies the ability to bind to multiple antigens, and the implications of that polyreactivity for the overall immune response.”
The new study found that these polyreactive antibodies tend to bind to the portions of the flu virus that are conserved, and that they are preferentially produced when the body encounters a novel flu strain. Importantly, their unique ability to bind to more than one antigen is potentially due to their flexibility; the antibodies themselves can slightly adjust their conformation, allowing them to imperfectly bind to multiple similarly-shaped antigens.
This means that polyreactive antibodies are broadly neutralizing due to their ability to attach to and block the portions of influenza virus that are similar across strains and from year to year. Polyreactive antibodies are therefore ideal candidates for developing a universal flu vaccine—one that can not only protect against common annual strains, but also novel influenza viruses, like the H1N1 strain seen during the 2009 pandemic.
The flexibility and strength of these polyreactive antibodies may make it seem like the ideal immune solution to protect against the flu, so why doesn’t the seasonal flu vaccine tend to trigger their production?
In the study, the investigators also found that these polyreactive antibodies can sometimes bind to the body’s own antigens, causing the polyreactive B cells to be destroyed to avoid an autoimmune response.
“What we’re seeing is that there’s this balance. Polyreactivity provides these beneficial features, like broader and better binding, but that comes at the cost of binding to self, which can cause issues,” said Guthmiller. “Our seasonal flu vaccine keeps calling back the same specific antibody response because it’s effective against these limited strains. To get these broadly neutralizing antibodies, like we’d want in a universal flu vaccine, we’ll need something very different, but now we know this has the potential to be self-defeating because of this self-binding.”
These results speak to the challenge of developing such a vaccine. “We already know it is difficult to target influenza in a universal fashion,” said Patrick Wilson, Ph.D., a professor of medicine at UChicago. “For better or worse, this paper provides important insights into properties of antibodies that can more universally target many influenza strains.”
Source: Read Full Article
