
As we’ve seen during the COVID-19 pandemic, serious infections sometimes trigger an excessive inflammatory reaction that does as much harm—or more—than the infection itself. New research at Boston Children’s Hospital and Brigham and Women’s Hospital suggests a potential way to block this hyperinflammation response by repurposing or modifying an existing drug.
The findings could potentially lead to a new treatment not just for COVID-19, but also for other life-threatening inflammatory conditions like sepsis and acute respiratory distress syndrome (ARDS) that currently have no specific treatment.
NETs, COVID-19, and inflammation
COVID-19, sepsis, and ARDS have something in common: All of them involve neutrophil extracellular traps, or NETs.
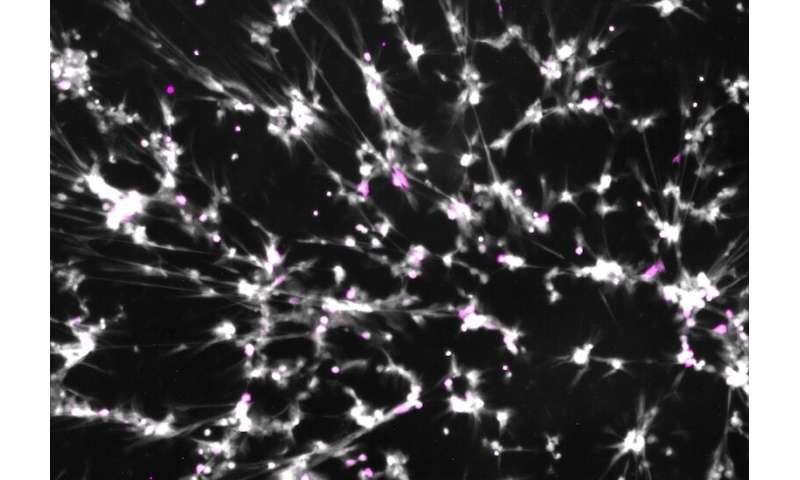
So what are NETs? They’re webs of DNA and toxic proteins that neutrophils, first-responder cells in the immune system, spew out to entrap bacteria or viruses, in a last-ditch attempt to contain the infection. (The neutrophils themselves, having lost their DNA, die in the process.)
“NETs are the final step,” says Ivan Zanoni, Ph.D., an immunology researcher at Boston Children’s and co-senior investigator on the study with Jeffrey Karp, Ph.D., of Brigham and Women’s. “If NETs appear, it suggests that other means of fighting the infection have failed. Neutrophils get the signal, “Give it everything you have.'”
But there’s a cost to making NETs. A growing body of research shows that the formation of too many NETs can lead to dangerous levels of inflammation, to blood clots such as those found in sepsis and severe COVID-19, and to direct tissue damage like that seen in severe lung infections and ARDS.
Preventing neutrophil extracellular traps from forming
The new study, led by Zanoni, Karp, and first author Valentina Poli, Ph.D., of Boston Children’s, suggests a way of curbing NETs and blocking potentially fatal inflammatory reactions. In the journal iScience, the researchers show that a drug called ricolinostat interferes with an early step involved in NET formation in neutrophils from both mice and humans and in three mouse models.
To form NETs, neutrophils first have to release their own DNA. This requires a specific group of enzymes called histone deacetylases (HDACs). These help open up the packaging around the DNA, known as chromatin. Ricolinostat, an HDAC inhibitor, blocks two classes of HDACs, class I and IIb.
“If you inhibit HDACs, you cannot open chromatin,” says Zanoni.
And if chromatin can’t open, the neutrophil cannot release its DNA and NETs cannot form. In the three mouse models—viral pneumonia, bacterial pneumonia, and a model of septic shock—the drug decreased NET formation and dampened inflammation. It protected lung function in the pneumonia models and reduced the harm caused by septic shock, appearing to reduce blood clot formation.
Working toward a clinical trial
Ricolinostat is currently in clinical trials for several cancers and for peripheral neuropathy in diabetes. Since it’s already gone through preclinical testing, Zanoni and Karp are looking to get it into clinical trials for severe inflammatory conditions. Zanoni’s lab has one modified version of ricolinostat that is also looking promising for blocking NET formation.
“Our work has potential to immediately help with COVID-19 to dampen the inflammatory response and turn it into something relatively harmless like a mild cold,” says Karp. “Inhibiting NETs represents a new therapeutic strategy for pulmonary diseases, autoimmune diseases like rheumatoid arthritis and systemic lupus erythematosus, diabetes, and cancer.”
Source: Read Full Article
