For the fourth summer in a row, Americans are experiencing a COVID-19 surge, this one marked by a rise in hospital admissions, emergency room visits, test positivity rates and wastewater data.
The good news: It’s unlikely that most cases will be severe or that the surge will be long-lasting, experts say.
The U.S. Centers for Disease Control and Prevention is reporting a rise in testing, though lab testing is not at the levels it was before the public health emergency ended in May.
“I do see some early signs that we are heading into another wave. Of course, we don’t know what lies ahead. So, it may yet peter out,” Caitlin Rivers, an assistant professor in the Department of Environmental Health and Engineering at the John Hopkins Bloomberg School of Public Health, told CNN.
“It doesn’t seem to be driven by a new variant, which I find encouraging,” Rivers added.
Gene sequencing company Helix has seen cases rise 30% to 40% since June, CNN reported. The company has been helping the CDC track gene changes of the COVID virus.
Numbers were at low levels before the recent rise, noted Shishi Luo, associate director of bioinformatics at Helix.
“When we look at our data, we have noticed that since late June to the beginning of July and probably through now, there has been a mild uptick in cases and these are based on samples sourced from pharmacy-based testing and also from health system-based testing,” Luo told CNN.
The reason for the rise may be that people are traveling more this summer and also meeting up indoors, where there is air conditioning because of heat waves.
Immunity has also waned over time. Most Americans have not had a COVID booster in a long time, CNN reported.
“Waning immunity clearly is going to play a role in all of this, and we’ve seen this over and over again, is the further out you get, even while there still is some protection against death and serious illness, waning immunity could be important in terms of the number of people who get sufficiently ill to require hospitalization,” Michael Osterholm, an infectious disease expert who runs the Center for Infectious Disease Research and Policy at the University of Minnesota.
Osterholm suggests getting the new booster for the XBB variant when it comes out in September.
“I want to get the new booster,” Osterholm said. “I think the evidence is that the protection of the previous bivalent booster has been reduced over time. So that if you get it now, though, that’ll hold you back time-wise from getting the new booster that hopefully will be out in the next 60 to 80 days.”
“I could get infected in that time period. But I really think that that vaccine is going to be a much better vaccine in terms of long-term protection, so I want to get it as soon as it comes out,” Osterholm said.
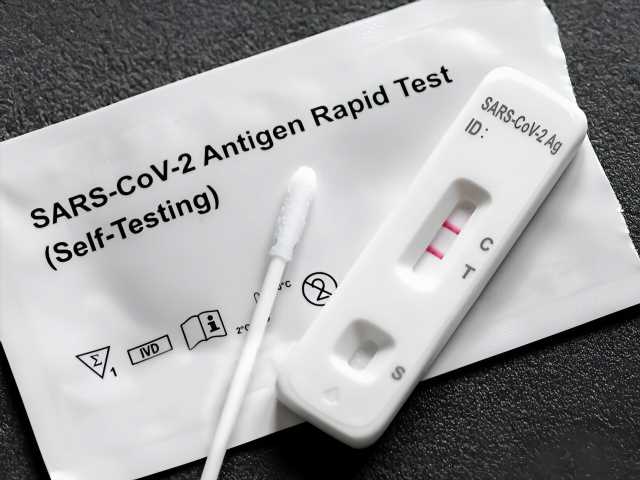
Ways to help prevent infection from spreading include testing as soon as you can if you feel ill or are planning to be in a crowded area.
Rivers said she’s not wearing a mask in public while cases are still low, “but if I’m traveling on an airplane or I’m getting on the metro, I would definitely want my mask on.”
Meanwhile, wastewater data is providing a consistent view of transmission trends.
Despite the rise, there are about one-third the concentration of coronavirus particles in sewage samples this year compared to last year, according to data from biotechnology firm and CDC partner Biobot Analytics.
The virus amount is also growing much more slowly than it did a few weeks ago, Newsha Ghaeli, president and co-founder of Biobot, told CNN.
“I wouldn’t say that in every instance a plateau has immediately led to a downturn. But we do typically see decreases once we hit a plateau,” she said.
In addition to COVID, CDC data suggests that adenovirus, norovirus and rotavirus are circulating at much higher levels this summer than last year, further muddying the picture for Americans.
More information:
The World Health Organization has more on COVID-19.
Copyright © 2023 HealthDay. All rights reserved.
Source: Read Full Article