Race—a social construct—is highly unreliable as a predictor of biologic variation across populations. Mounting evidence showing that race is not biology has called into question the use of many diagnostic tests and treatment approaches that still rely on outdated notions of race as a way to capture differences in biology and physiologic function across individuals with different genetic ancestries.
Recently, a task force convened by the National Kidney Foundation and the American Society of Nephrology recommended a new race-free clinical calculator to estimate how well a person’s kidneys work. For decades, the formula to calculate kidney function has included race as one of several variables.
The task force has recommended three race-free equations, each one including different combinations of variables, including as a patient’s age and sex plus levels of creatinine (a waste by-product filtered by the kidneys) and cystatin-C (a protein released by cells and broken down by the kidneys).
But what will the adoption of these new formulas mean in practical terms for patients and for the clinicians who treat them?
This is the question that for several years has occupied the attention of a research team led by investigators at Harvard Medical School. The team’s latest report, published Nov. 11 in the Journal of the American Society of Nephrology, caps a series of studies and represents the most comprehensive analysis yet on the effects of new calculators for kidney-function assessment.
The newly published study estimates how the widespread adoption of one of the three race-free equations could change patterns of diagnosis, disease classification, and treatment decisions.
The team said that removing race from kidney calculators is a step in the right direction and that the new findings should arm patients and clinicians with the knowledge necessary to clarify diagnostic decisions and inform treatment choices.
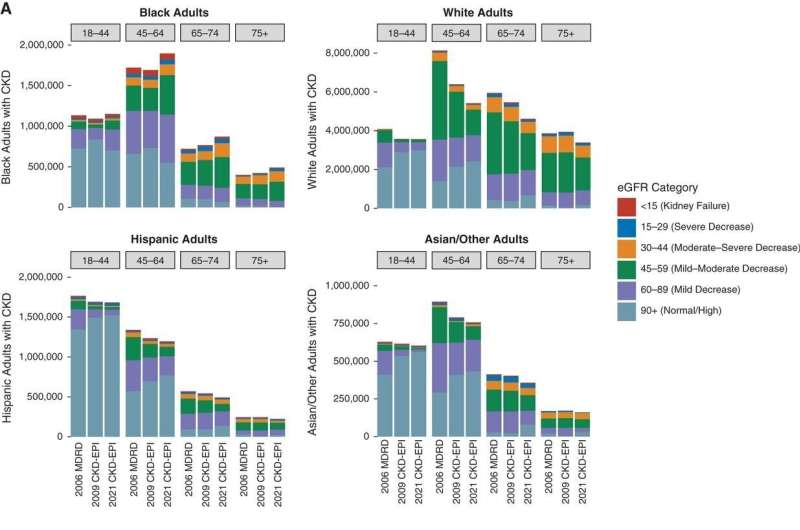
According to the analysis, the widespread adoption of the new formula based on a patient’s age, sex, and creatinine level is expected to:
- Lead to 434,000 new diagnoses of chronic kidney disease among Black individuals and reclassify 584,000 Black patients to a more advanced disease stage.
- Eliminate kidney disease diagnoses for 5.5 million non-Black adults and reclassify 4.6 million non-Black adults as having a less advanced stage of chronic kidney disease.
- Expedite diagnoses and referrals to specialized care for newly diagnosed Black individuals, including earlier evaluations for kidney transplantation and coverage by Medicare and other insurance.
- Identify some 222,000 Black adults who may require dose reductions or contraindications for certain medications, including drugs for high blood pressure, heart disease, diabetes, seizures, chronic pain, or bacterial infections. Conversely, some 1.47 million non-Black adults may no longer require dose adjustments for such medications.
Study lead author James Diao, a fourth-year medical student at HMS, and senior author Arjun Manrai, assistant professor of biomedical informatics in the Blavatnik Institute at HMS, spoke with HM News about the implications of the findings and the broader significance of race-free kidney-function testing.
Harvard Medicine News: You have done a series of studies on race and kidney function. What sparked your interest in this area?
Manrai: Our lab is focused on the application of machine learning and statistical modeling to clinical decision-making, including understanding how the use of genomic data and common laboratory biomarkers such as creatinine should guide clinical decisions. Caring for diverse populations has been a major area of interest for us over the past decade. Some of our key initial work in this area includes our study of genetic variant misclassification for inherited heart disease across populations.
I am particularly sensitive to this topic. My mother, who passed away several years ago, would see a nephrologist to have her kidney function measured. She once received a report from the laboratory saying that if the patient was African American, they would have this kidney function, and if they were non-African American, they would have that kidney function. My mother asked her nephrologist what her kidney function value would be as an Indian American. He told my mom he’d average the two values for Black and non-Black individuals. This is what “precision” medicine looks like in the absence of guidance and clarity. This example also underscores that race is often operationalized as a crude, imprecise, and problematic label.
Diao: We have been interested broadly in equity and representation in health care and how constructs like race get codified in clinical guidelines and common clinical equations. Using race in this way often reifies the faulty, outdated notion of race as biology and destiny. We saw the changes to kidney-function tests as an opportunity to use data analysis to inform this conversation and help guide policy.
HM News: Your analysis forecasts significant changes in care as a result of adopting one of the new formulas. What is the message for hospitals?
Manrai: First of all, removing race from kidney-function equations is absolutely the way forward. At the same time, it’s important to understand how this change might affect patients in your clinic and in your hospital. If you are a hospital administrator, you should be aware that changes to guideline-recommended care may result from the new formula, including changes to chronic kidney disease diagnoses, kidney waitlist and donation eligibility, and medication changes for different patient populations. This may help inform resource allocation and planning, and it also points to the importance of follow-up confirmatory testing as needed.
HM News: What are the implications for patients and the physicians who care for them?
Diao: At the individual patient level, it’s important to keep in mind that minor shifts in kidney function should be anticipated as a result of the new formula, but any significant changes in a patient’s kidney function would require the physician to probe further to determine how much of it is coming from the change in the equation itself and how much is due to an actual change in the patient’s disease and kidney status. Is the change larger than what would be predicted from the change in the formula alone?
If so, then it’s probably not coming from the equation itself. The equation provides an estimate, not a direct measure, of kidney function, but there are a number of confirmatory tests that may be valuable, including the use of additional biomarkers or a direct measurement of kidney function. Of course, clinicians will always contextualize the value of a test by using other patient-specific clues that emerge during the exam, such as the presence or absence of symptoms suggestive of worsening kidney function.
HM News: Race-based formulas are used in other clinical tests beyond kidney function. What is the way forward?
Manrai: Race has been deeply embedded in many areas of medicine and is not unique to kidney-function tests, but we are seeing a growing recognition that race is imprecise and problematic. I think the use of race will be challenged, reconsidered, and eventually removed from many other areas of medicine.
There are many lessons we learned from our work with the kidney-function equation. The kidney community did a number of things right, including forming a task force built on diverse perspectives and areas of expertise—from nephrologists, epidemiologists, and genetics experts to sociologists, anthropologists, and historians of medicine—along with the inclusion of patient representation.
As other professional medical societies look to modify race-based clinical tests, they can learn from this transparency and the deliberate incorporation of diverse perspectives.
The second big lesson is that data and evidence have to be injected into these debates, ideally from the very beginning. Long term, we need to identify better, more reliable biomarkers that explain human variation. We need to move beyond crude proxies and toward a much more precise understanding of physiologic variation, including both better molecular biomarkers and a much richer understanding of the patient’s environment.
More information:
James A. Diao et al, National Projections for Clinical Implications of Race-Free Creatinine-Based GFR Estimating Equations, Journal of the American Society of Nephrology (2022). DOI: 10.1681/ASN.2022070818
Journal information:
Journal of the American Society of Nephrology
Source: Read Full Article
