TOPLINE:
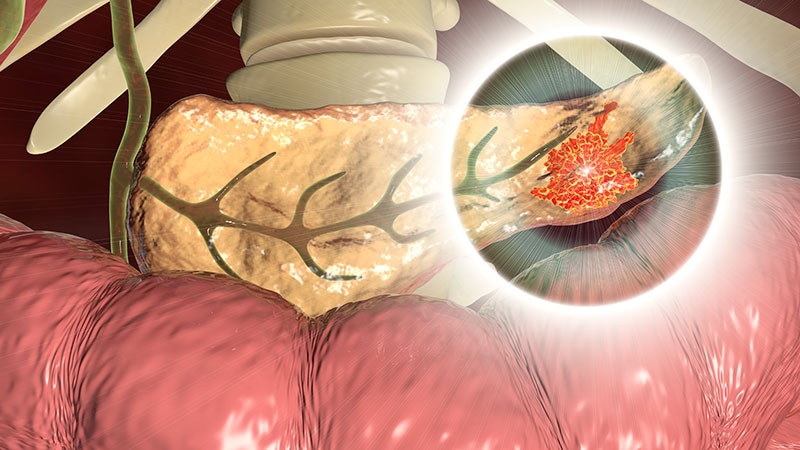
An artificial intelligence (AI) model shows potential for detecting early-stage, “hidden” pancreatic cancer on scans of asymptomatic individuals, paving the way for surgical intervention and cure, new research suggests.
METHODOLOGY:
-
The researchers utilized a diverse dataset of 3014 CT scans: 1105 diagnostic CT scans with pancreatic ductal adenocarcinoma (PDA) and 1909 control CT scans.
-
Of the total, 696 diagnostic CT scans with PDA and 1080 control CT scans were used as an AI model training subset, and 409 CT scans with PDA and 829 control CT scans were used as an intramural hold-out test subset.
-
The model was also tested on a simulated cohort that evaluated the risk for PDA in new-onset diabetes; multicenter public datasets (194 CT scans with PDA and 80 controls); and a cohort of 100 prediagnostic CT scans, incidentally acquired 3-36 months prior to PDA being diagnosed, and 134 controls.
TAKEAWAY:
-
The model correctly classified 360 CT scans with PDA (88%) and 783 control CT scans (94%) in the intramural test subset. The mean accuracy was 0.92, the area under the receiver operating characteristic (AUROC) curve was 0.97, sensitivity was 0.88, and specificity was 0.95.
-
On heat maps, activation areas overlapped with the tumor in 350 of 360 CT scans (97%).
-
Performance was high across tumor stages, with sensitivities of 0.80, 0.87, 0.95, and 1.0 on T1 through T4 stages, respectively. Performance was comparable for hypodense vs isodense tumors (sensitivity of 0.90 vs 0.82, respectively), patient demographics, CT slice thicknesses, and vendors.
-
Findings were generalizable on both the simulated cohort (accuracy, 0.95; AUROC curve, 0.97) and public datasets (accuracy, 0.86; AUROC curve, 0.9).
-
Occult PDA was detected on prediagnostic CT scans at a median 475 days before clinical diagnosis. Accuracy was 0.84, AUROC curve was 0.91, sensitivity was 0.75, and specificity was 0.9.
IN PRACTICE:
“Artificial intelligence model could mitigate the inadequacies of imaging and the diagnostic errors in interpretation, which often contribute to delayed diagnosis of pancreas cancer. In combination with emerging blood-based biomarkers, such a model could be evaluated to screen for sporadic cancer in ongoing trials of high-risk cohorts such as the Early Detection Initiative (NCT04662879).”
SOURCE:
Panagiotis Korfiatis, PhD, of Mayo Clinic, Rochester, Minnesota, led the study, which was published online August 30 in Gastroenterology.
LIMITATIONS:
The retrospective design is prone to selection bias. Results are presented dichotomously as either cancer or control. These are preliminary insights, and prospective clinical trials that incorporate epidemiological risk factors and emerging blood-based biomarkers are needed to further evaluate the model’s performance.
DISCLOSURES:
The research was supported by the National Cancer Institute of the National Institutes of Health, the Centene Charitable Foundation, and the Champions for Hope Pancreatic Cancer Research Program of the Funk Zitiello Foundation. One author received an institutional research grant from Sofie Biosciences and Clovis Oncology, is on the BlueStar Genomics advisory board (ad hoc), and is a consultant for Bayer Healthcare LLC, Candel Therapeutics, and UWorld. The remaining authors report no relevant financial relationships.
Follow Marilynn Larkin on X: @MarilynnL
For more news, follow Medscape on Facebook, X (formerly known as Twitter), Instagram, and YouTube
Source: Read Full Article