New, real-world evidence demonstrating that the KidneyIntelX bioprognostic test resulted in changed clinical decision making for patients in the early stage of diabetic kidney disease (DKD) being cared for within the Mount Sinai Health System’s Population Health Ambulatory Pharmacy and Condition Management programs has been published in the Journal of Primary Care & Community Health. The majority of patients were being treated by their primary care physician.
Prediction of risk for kidney disease progression in early-stage DKD is often not assessed at the primary care level, resulting in more than 50,000 individuals per year with diabetes progressing to kidney failure, dialysis or a kidney transplant. By integrating an easily interpretable, accurate prognostic tool that assigns a risk score for progressive decline in kidney function, KidneyIntelX enables providers to act earlier to slow or stop the progression to kidney failure.
“The data is greatly encouraging for millions of early stage 1–3 DKD patients where we lack patient-specific risk assessment tools to adjust appropriate care. Utilizing KidneyIntelX to identify which patients can most benefit from guideline-based therapies such as SGLT2 inhibitors, more education on diabetes and CKD, and referrals to specialists such as dieticians, diabetologists, and/or nephrologists, is an opportunity to swing the pendulum from suboptimal to optimal care,” said Robert Fields, MD, MHA, executive vice president and chief population health officer for the Mount Sinai Health System.
According to Michael J. Donovan, Ph.D., MD, chief medical officer at Renalytix, “The impacts of KidneyIntelX early risk assessment, even at this interim six-month time point, are very encouraging that we can proactively move to control cost and outcomes in diabetes and kidney disease. Enabling primary care physicians to recognize risk and clinically manage patients with DKD can potentially eliminate unnecessary events from uncontrolled disease progression, including kidney failure and dialysis. We look forward to continuing published data releases at the one-year mark.”
Key points from the prospective study:
- The study was conducted in collaboration with the Mount Sinai Health System’s Population Health Ambulatory Pharmacy and Condition Management programs and included 1,686 patients seen by 75 providers at 20 clinical sites.
- The RWE study demonstrated that patients with early-stage DKD and a high risk KidneyIntelX score received higher frequency of clinical management visits, introduction to guideline-recommended medications, and specialist referral for disease management compared to those who were identified as low or intermediate risk patients.
- The risk breakdown of the RWE study population was similar to the clinical validation cohort (high risk 12% vs. 17%, intermediate risk 40% vs. 37%, and low risk 48% vs 46%, respectively).
- Frequency of follow up visits: 53% of all KidneyIntelX high risk patients had a follow-up visit within 1-month of their KidneyIntelX test and 57% had action taken (medication change or referral) within three months, compared to 13% and 35%, respectively, for low risk patients.
- Medication management: When evaluating new or modified prescriptions for hypertension at six months, both ACEi and ARBs achieved a greater than 20% change in patients with hypertension in the high risk group vs. the low risk group. Medication management for use of SGLT2 inhibitors was even more pronounced; 25% of patients in the high risk group received new SGLT2i prescriptions vs. 7% in the low risk group, a 4.5-fold increase. Thus, KidneyIntelX enabled physicians to take guideline-recommended clinical actions in high risk, early stage (stage 1–3b) diabetic kidney disease patients.
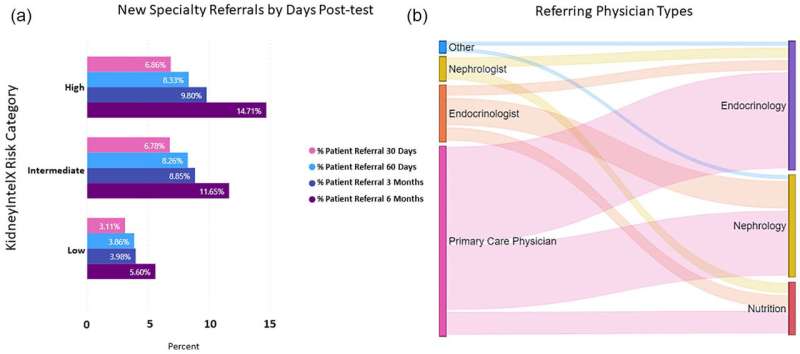
- Specialist referrals: New referrals by risk group were 6% for low risk, 12% intermediate risk and 15% high risk.
Source: Read Full Article
