A type of white blood cell previously known only as a helper in the immune system appears also to be the instigator of the body’s defenses against cancerous tumors. The discovery could lead to more effective cancer immunotherapy, a promising treatment which uses the body’s own immune system, rather than radiation, to attack cancer cells.
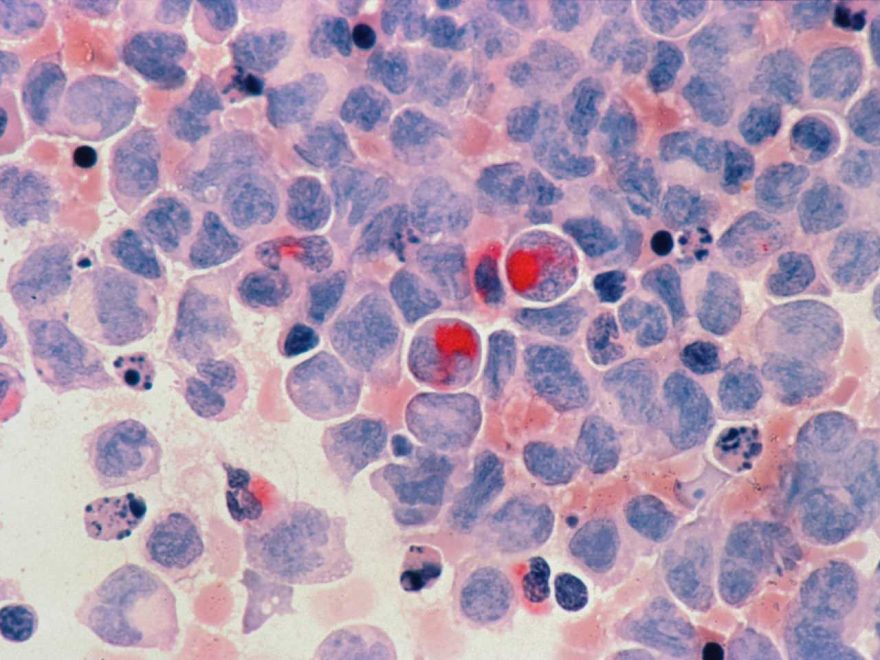
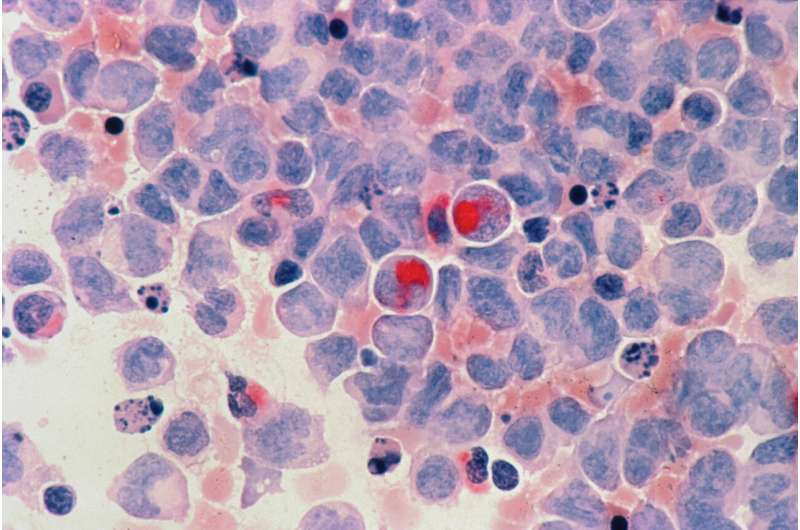
In an animal study, Washington State University researchers found that a population of T cells called CD4-positive helper T cells helped start a chain of antitumor immunity defenses that allow killer cells to better infiltrate melanoma and breast cancer tumors. T cells belong to a class of white blood cells known as lymphocytes which move throughout the body’s lymphatic system.
Many previous studies, and current immunotherapies, have focused primarily on the role of one-type of killer cells, called CD8-positive T cells. Yet, less than 20% of patients respond to those therapies and the initiating role of the CD4-positive helper cells could make those therapies better, said Hui Zhang, lead author on the study published in the Journal of Immunology.
“One of the most challenging parts of current cancer immunotherapy is the low response rate,” said Zhang, a WSU assistant professor of pharmaceutical sciences. “The lack of knowledge of how to enhance lymphocyte infiltration into the tumor hampers the success of improving the response rate to cancer immunotherapy. Our finding shows promise in solving this problem.”
Cancer is the second leading cause of death both nationally and worldwide. Currently, surgery, chemotherapy and radiation therapy are the conventional approaches to cancer treatment. However, those approaches cannot cure many cancers because some become metastatic, spreading from the primary tumor throughout the body, and certain cancer stem cells can become resistant to chemotherapy and radiation.
A relatively new treatment, immunotherapy has shown promise in curing a range of cancers, but only a relatively low number of patients respond to it. Zhang’s research team hopes to change that with the knowledge of the mechanisms that help start the body’s immune defenses.
The immune system has two types of killer cells: the CD8-positive T cells, and so-called “natural killer” cells. Both can attack virally infected cells and cancer cells.
Natural killer cells are innate and roam around the body. They act as the first line of defense in our immune system but cannot recognize specific antigens—toxins or other foreign substances in the body—on their own. After the natural killer cells start to work, the CD8-positive T cells, which can recognize specific antigens, arrive. While CD8-positive T cells and their mechanisms have been well studied and are used in current immunotherapies, not much is known about how to activate natural killer cells’ antitumor function.
Using genetic knock-out mice experiments, Zhang’s group found evidence that a certain type of CD4-positive T cells, called tissue-resident memory T cells, may be critical in activating those first lines of natural killer cell defenders. Their experiments showed that they were effective against both melanoma and breast cancer tumors.
“We found that this specific population of CD4 T cells were the key player to initiate the antitumor immunity,” said Zhang.
The specific CD4 T-cells together with the natural killer cells not only killed tumor cells and controlled tumor progression but also enhanced infiltration of other white blood cells, or lymphocytes, into the tumor.
In future studies, the researchers plan to continue to investigate the precise cellular and molecular mechanisms of this antitumor immunity—first in mice to develop an effective cancer immunotherapy. Then, the team hopes to move on to clinical trials in human subjects.
Source: Read Full Article