Fiji’s national vaccine program against pneumonia, a serious lung condition, and rotavirus, a common disease which causes severe diarrhoea and vomiting, has reduced illness and death, new research shows.
The University of Melbourne-led research team, which worked with the Fiji Ministry of Health and Medical Services, says the results underline the importance of vaccines and how they can potentially reduce the impact of viruses such as COVID-19.
Published in The Lancet Regional Health—Western Pacific, the first study looked at Fiji’s national rotavirus vaccine program five years after it became the first independent Pacific island country to introduce the vaccine in 2012, and one of few in the Asia-Pacific region.
Morbidity (disease or symptom) and mortality (death) due to rotavirus and all-cause diarrhoea in Fiji fell in those aged two months to 55 years. Rotavirus diarrhoea admissions at the largest hospital among children aged under five fell by 87 per cent.
Lead researcher Professor Fiona Russell, of Murdoch Children’s Research Institute and the University of Melbourne, said the findings underlined a wider effort to introduce the vaccine across the Pacific.
“The high uptake means the vaccine was acceptable to the children and their carers,” Professor Russell said.
“It showed sustained effectiveness, working in vaccinated children and helping to prevent other members of their household falling ill.”
Rotavirus is severely contagious and the most common cause of diarrhoeal disease among infants and young children. It can cause death in extreme cases.
In October 2012, the Fiji Government introduced a rotavirus vaccine into the national immunisation schedule at six and 14 weeks with the Australian Department of Trade and Foreign Affairs’ support. National coverage estimates were 85, 91, 94, 93 and 98 per cent in 2013, 2014, 2015, 2016 and 2017, respectively.
“Fiji is the first Pacific island country to show a decline in the burden of rotavirus diarrhoea, and all-cause diarrhoea admissions in people of all ages and mortality in children after rotavirus vaccine introduction,” Professor Russell said.
“These reductions were most likely due to the vaccine as rotavirus diarrhoeal outbreaks remained blunted for the five years after vaccine introduction. While improved outpatient management practices may have contributed to the decline in diarrhoea, the temporal relationship to vaccine introduction is compelling.”
At the same time in 2012, the Fiji Government introduced a routine infant immunisation schedule for ten-valent pneumococcal conjugate (PCV10) vaccine using three primary doses and no booster dose.
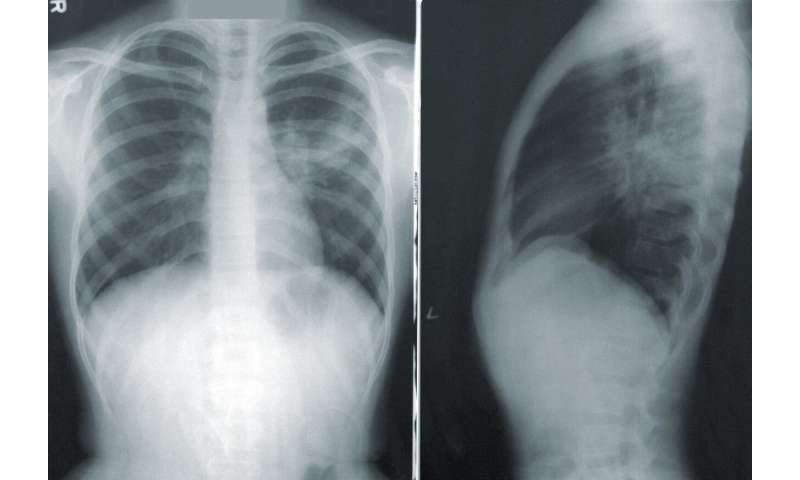
Published in The Lancet Global Health, this study looked at hospital admission rates for children presenting with pneumonia from January 2007—December 2017 at three Fiji public tertiary hospitals.
Five years after the vaccine was introduced, hospital admissions for all-case pneumonia had fallen for children aged 24-59 months.
Mortality was down by 39 per cent among children aged two-24 months who were admitted to hospital with all-case pneumonia, bronchiolitis, and asthma.
Professor Russell said the second study was the first in a middle-income Asia-Pacific region country to show the effect of PCV10 vaccine and supported its introduction for children in other low and middle-income countries in that region.
“These results provide supportive evidence of the probable benefits of PCV10 in reducing pneumonia in children in Fiji,” Professor Russell said.
Source: Read Full Article
